Top Warning Signs of Deep Venous Reflux
Venous Reflux Disease (VRD), also known as Chronic Venous Insufficiency (CVI) probably isn’t a topic you discuss over the dinner table. The fact is, it’s more common than you might realize. Women are the largest targets for Venous Reflux Disease. 40% of women will develop it, usually between 40 and 49 years of age.
Men are at less of a risk for developing this condition, but they still should be aware of the symptoms of Venous Reflux Disease. This article will discuss Deep Venous Reflux, which impacts deep veins rather than superficial veins.
What is Venous Insufficiency?
Chronic venous insufficiency results from the inadequate blood flow back to the heart through your veins. There are a variety of causes for venous insufficiency but the most common include incompetent valves in your veins or some other blood flow obstruction. Chronic Venous insufficiency increases your risk factors for developing a clot. These clots usually form in the leg and are called a Deep Vein Thrombosis (DVT) if it develops in a vein below the muscle facia. This is a life threatening condition because the clot may dislodge and travel into the lungs. If it does, there is a potential that you will develop a pulmonary embolism.
Another term you should know is Venous Stasis Ulcer (VSU). Chronic venous insufficiency often results in the pooling of blood in the pelvic and lower extremities. This increased blood volume causes an increased venous pressure in the surrounding tissue and the constant venous pressure pushes fluids from your veins into the surrounding tissues. If this process continues, it can cause a venous stasis ulcer. The ulcers are difficult to heal and could be debilitating.
Common Risk Factors for Venous Reflux Disease
There are common risk factors for venous insufficiency. Many of them are related to women. Venous reflux disease usually affects men over 50 years of age.
Here are the increased risk factors for Deep Venous Reflux:
- History of blood clots
- Obesity
- Pregnancy
- Cancer
- Smoking
Common Warning Signs of Venous Reflux
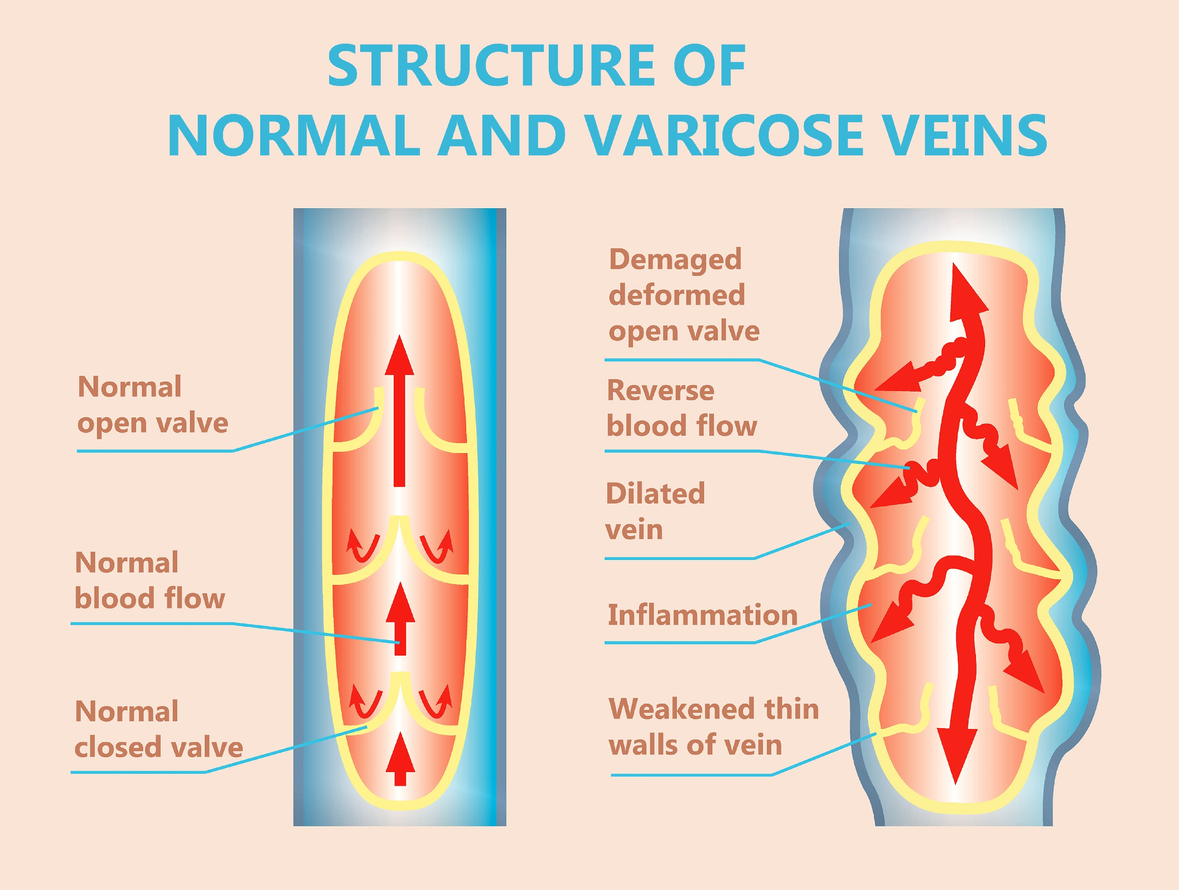
Venous reflux occurs when the veins are blocked or damaged. The veins that transit the leg pump blood from the thighs, shins, and feet back to the heart.
When these veins become impaired, blood will begin to pool in the feet, toes, or legs. The longer this condition occurs, the thinner and weaker the veins will become. It’s important to know the warning signs that venous reflux may be developing in your legs.
8 Signs You May Have Venous Insufficiency
Here are some signs that you may have Venous Insufficiency.
#1 Swelling in the Legs or Ankles
Venous insufficiency will commonly cause the legs or ankles to swell, called edema. The swelling is caused by the pooling of blood. Patients may notice that the swelling extends to the thigh area. This swelling is often painless.
Anyone who takes the following medications may notice swelling:
- Calcium channel blockers
- MAO inhibitors
- Antidepressants
- Estrogen
#2 Feeling of Heavy or Achy Legs
When blood flow to the legs decreases because of venous insufficiency, patients may sense that their legs feel heavy or ache. Some of the other symptoms may include:
- Cramping
- Tingling
- Itching
- Pain
Another warning sign is if the conditions listed above worsen when standing or if you feel an unusual tightness in your calves. Doctors recommend laying down and elevating your legs if these symptoms occur.
#3 Leg Ulcers
When venous insufficiency is not treated, it may lead to leg ulcers. These may also be called venous stasis ulcers. The ulcers will manifest as open wounds that are slow to heal. If you have an open wound on your leg that has not healed in two weeks, this is a warning sign.
The location of leg ulcers resulting from venous reflux is usually near the ankle, inside the leg. Look for signs that the skin surrounding the ulcer is hard or discolored. You know the ulcer is infected if pus develops.
#4 Varicose Veins
You will see varicose veins develop just below the skin on the legs. This is a common warning sign of venous insufficiency. Look carefully to see if the veins have increased in size and are twisted. Itching of the enlarged veins is another warning sign.
Varicose vein complications include aching, itching, and pain. Be aware that in conjunction with the varicose veins, if there is swelling in the legs, discoloring, or sores, you need to see a doctor and determine if you have venous insufficiency.
#5 Leg Cramps
If you have new or sudden severe leg cramps, this may be a warning sign of venous insufficiency. The cramps are caused by the contraction of leg muscles, usually in the calf muscle. The muscle may be briefly immobilized and may be accompanied by burning and throbbing.
Cramps associated with venous insufficiency may take place in the thighs and feet. Some people report that the cramps present themselves in the evening. Doctors don’t understand how leg cramps coincide with venous insufficiency. It should be ruled out by a doctor that they are not a symptom of CVI.
#6 Leg Pain Worsens When Standing
Leg pain can be caused by many factors. If the leg pain gets worse when standing, it may be a warning sign of venous insufficiency. If you have other factors with the increase in pain, such as a heavy sensation, throbbing, or aching, this increases the chance that you are experiencing CVI.
Be aware of an increase in any of these symptoms when you are standing in line at the store, when you are sitting down and then standing, or when you get out of bed in the morning.
#7. Skin Around Legs or Ankles Thickens
If you are unaware that you have venous insufficiency, and it is left untreated, the skin around your legs and ankles could thicken. This thickening may be combined with swelling and inflammation.
When the skin thickens around the legs and ankles, you will experience pain when putting on shoes and exercising. You may notice varicose veins around the thickened skin accompanied by swelling in the legs and ankles, all signs you should be checked for CVI.
#8. Changes in Skin Color
A warning sign of venous insufficiency may be a change in skin color. This change is triggered by a build-up of pressure in the veins of the lower legs. Small capillaries can burst, which may cause the skin to turn reddish-brown. You may first notice the color change around the ankles, but it may spread to other parts of the legs.
This change of color may also be a sign of an active blood clot. If you notice a change in skin color, call your doctor immediately.
Knowing the symptoms and signs of venous insufficiency is important to catch the disease early and increase your chances of healing. The disease impacts the walls and valves of your veins. Instead of pumping back to your heart, blood starts to pool. Venous insufficiency develops when the veins no longer pump blood back to the heart properly.
If you experience varicose veins, swelling, pain, aching, or a heavy feeling in your legs, contact your doctor. Other symptoms of venous insufficiency may include sores around your ankles or a change in skin color. If it hurts to stand or you have any unusual feelings in your legs or ankles, check that you are not in danger of CVI.
What to expect from Vascular Specialists at CVM?
At the Center for Vascular Medicine, our mission is to help patients with their vascular diseases in a cost-effective and compassionate manner. We specialize in the diagnosis and treatment of venous and arterial diseases in the legs, feet, and pelvis. Our world-class vascular providers are the most experienced in the specialty and work with patients to develop a treatment plan that is custom-tailored to their unique situation.
Typically, this process involves an initial consultation with a possible ultrasound scan at one of our facilities. After reviewing the results of your scan and obtaining a thorough medical history, our providers will discuss the results with you and help you decide on the next steps.
Call to schedule at (301) 486-4690 or fill out a request to consult form.

