What is Deep Vein Thrombosis?
Deep vein thrombosis (DVT) is a severe condition that demands prompt medical attention. It occurs when a blood clot, or thrombosis, forms in a deep vein, usually in the legs. These veins are part of the vascular system that returns blood to the heart. When a clot develops in these veins, it can obstruct blood flow and lead to severe complications.
In severe cases, the blood clot can break loose and travel through the bloodstream, known as embolization. If the clot reaches the lungs, it can cause a life-threatening condition called a pulmonary embolism (PE). Immediate medical attention is crucial, although many clots dissolve on their own.

Visit one of our Center for Vascular Medicine Locations for a comprehensive diagnosis.
Am I At Risk for Deep Vein Thrombosis?
Several factors can increase your risk of developing DVT. Understanding these risks can help you take preventive measures and seek early treatment.
Common risk factors for deep vein thrombosis include but aren’t limited to:
- Prolonged immobility, including sitting for long periods, such as during travel or bed rest, can increase the risk of DVT.
- The CDC states that anyone traveling for more than four hours can be at risk.
- The risk of DVT increases with age, especially for those over 60.
- A family history of DVT or clotting disorders can elevate your risk.
- Obesity can increase pressure on your legs and pelvis veins.
- Previous surgery involving the legs, hips, or abdomen can lead to prolonged immobility, which can increase your risk for deep vein thrombosis.
- Medical conditions such as cancer, heart disease, and inflammatory bowel disease can increase the risk.
- Pregnancy increases the pressure in the veins of your pelvis and legs. This risk continues for up to six weeks postpartum.
- Hormone therapy, such as birth control pills or hormone replacement therapy, can increase blood clotting ability.
- Smoking affects blood clotting and circulation, increasing the risk of DVT.
Deep Vein Thrombosis (DVT) is a severe condition that can lead to significant health complications. However, there are several effective strategies to reduce your risk.
Stay Active and Exercise Regularly
Regular physical activity is one of the most effective ways to reduce the risk of DVT. Exercise helps promote healthy blood circulation and prevents blood from pooling in the veins, particularly in the legs.
Aerobic activities like walking, swimming, and cycling are excellent options for maintaining good circulation. Simple exercises like leg lifts, ankle circles, and calf raises can be done even while sitting to keep the blood flowing. Regular stretching can improve circulation and prevent stiffness, especially during long periods of sitting or inactivity. Some patients can exercise aerobic and strength training to support weight loss and muscle maintenance. Talk to your vascular specialist before starting any new exercise routine to ensure it’s right for you.
Remember to avoid long periods of inactivity as they can increase the risk of DVT. It's important to move regularly to keep your blood circulating. Take breaks every hour to stand, stretch, and walk around, especially during long flights or car rides. For those with a sedentary job, try incorporating simple desk exercises like leg stretches and ankle rotations. Wearing compression stockings can also help improve blood flow in the legs during long periods of sitting.
Maintain a Healthy Weight
Maintaining a healthy weight is crucial in reducing the pressure on your veins, particularly in the legs. Excess weight can increase the risk of DVT by putting additional strain on your vascular system. Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Be mindful of portion sizes to avoid overeating. Stay hydrated, as dehydration can thicken your blood, making it more prone to clotting. Ensuring you stay well-hydrated helps smooth blood flow and reduces the risk of clots forming. Aim for at least 8-10 glasses of water per day, and l limit sugary, caffeinated beverages and alcohol, as both can contribute to dehydration if consumed in excess.
Make Healthy Changes
Talk to your vascular specialist about resources to quit smoking. Smoking affects your blood circulation and increases the risk of clotting. Quitting smoking can significantly reduce your risk of developing DVT and improve your overall vascular health.
Follow Medical Advice
If you have risk factors for DVT, such as a previous history of blood clots, certain medical conditions, or genetic predispositions, it’s essential to follow your healthcare provider’s recommendations. Make sure to keep all your follow-up appointments, take any prescribed medications, and adhere to any other instructions from your healthcare provider.
Reducing your risk of developing deep vein thrombosis involves lifestyle changes, medical interventions, and preventive measures. Staying active, maintaining a healthy weight, staying hydrated, avoiding prolonged inactivity, quitting smoking, and following medical advice can significantly lower your chances of developing DVT. If you have any concerns or symptoms, consult a vascular specialist at Center for Vascular Medicine for a comprehensive evaluation and personalized care plan.
What are the Symptoms of Deep Vein Thrombosis?
Deep vein thrombosis is a medical emergency with the potential to be fatal. Some patients may not experience all the symptoms of DVT, and the symptoms can vary and may not always be apparent. Seek medical attention if you experience symptoms such as:
- Sudden, unexplained swelling in the leg.
- Pain in the leg, often described as cramping or soreness, usually worsens when flexing the foot.
- Redness and warmth in the affected area.
- The skin may appear red, purple, pale, or blue, particularly on the back of the leg below the knee.
- Confusion, disorientation, or dizziness accompanied by the above symptoms.

Symptoms of Pulmonary Embolism (PE)
If a blood clot travels to the lungs, causing a pulmonary embolism, you may experience:
- Sharp, stabbing chest pain that may worsen with deep breaths.
- Shortness of breath, difficulty breathing, or rapid breathing.
- A persistent cough that sometimes produces bloody or pink-tinged sputum.
Timely recognition and treatment of DVT and PE can save lives. If you have any concerns or notice any symptoms, do not hesitate to contact a healthcare professional or visit a vein clinic such as Center for Vascular Medicine. Early diagnosis and intervention are essential in managing DVT effectively and preventing severe complications. Your vascular health and well-being are paramount, and proactive measures can significantly impact outcomes.
High-Risk Patients with DVT
Inheriting a blood-clotting disorder. Some people inherit a disorder that makes their blood clot more easily. This condition, on its own, might not cause blood clots unless combined with one or more of the other risk factors.
Prolonged bed rest, such as during a long hospital stay, or paralysis. When your legs remain still for long periods, your calf muscles don't contract and help blood circulate, which can increase the risk of blood clots.
Injury or surgery. Injury to your veins or surgery can increase the risk of blood clots.
Pregnancy. Pregnancy increases the pressure in the veins of your pelvis and legs. Women with an inherited clotting disorder are at increased risk. The risk of blood clots from pregnancy can continue for up to six weeks after childbirth.
Birth control pills (oral contraceptives) or hormone replacement therapy. Both can increase your blood's ability to clot.
Being overweight or obese. Being overweight increases the pressure in the veins of your pelvis and legs.
Smoking. Smoking affects blood clotting and circulation, which can increase your risk of DVT.
Cancer. Some forms of cancer increase the amount of clotting factors in your blood. Some forms of cancer treatment also increase the risk of blood clots.
Heart failure. This increases your risk of DVT and pulmonary embolism. The symptoms caused by even a small pulmonary embolism are more noticeable because people with heart failure have limited heart and lung function.
Inflammatory bowel disease. Bowel diseases, such as Crohn's disease or ulcerative colitis, increase the risk of DVT.
A personal or family history of deep vein thrombosis or pulmonary embolism. If you or someone in your family has had one or both of these, you might be at greater risk of developing a DVT.
Age. Being older than 60 increases your risk of DVT, though DVT can occur at any age.
Sitting for long periods of time, such as when driving or flying. When your legs remain still for long periods, your calf muscles don't contract and help blood circulate. Blood clots can form in the calves of your legs if your calf muscles don't move for long periods.
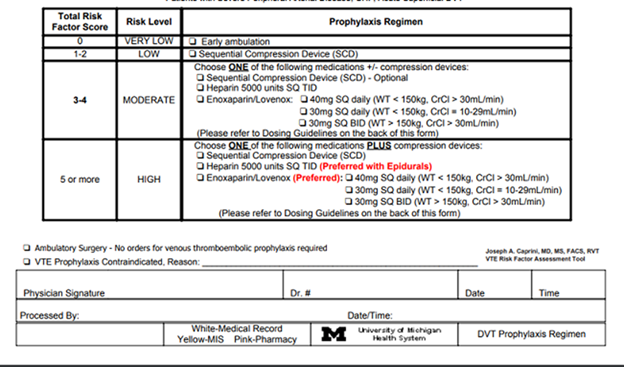
Caprini Model used before surgery helps determine a patient's risk of developing a DVT
In 2005, Dr. Joseph Caprini created the “Caprini Model” to help physicians determine if patients are at risk of developing DVT. Today, this is widely used by vascular specialists to help determine patients' risk of developing DVT after surgery.
The chart below shows a portion of the comprehensive assessment used by our medical professionals to determine DVT risk after surgery.
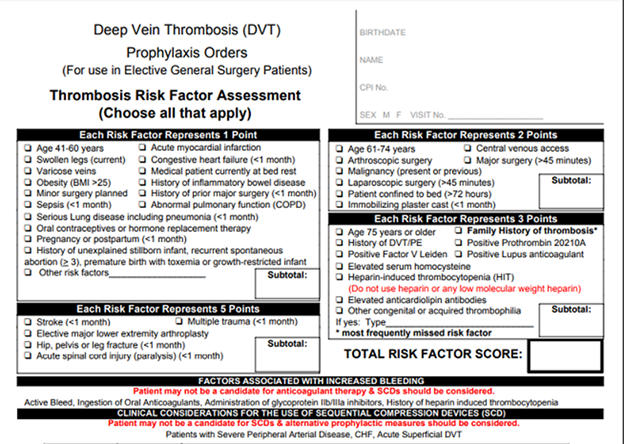
The risk of DVT increases with the presence of more risk factors. CVM’s vascular specialists determine a score of 0-2, to be of low risk. Patients with a risk score of 3 or more should consider anticoagulation (anti-blood clot) medication to decrease the risk of developing DVT. In addition, compression therapy may be recommended. You can also read How do you know if you have blood clot after surgery?
How is Deep Vein Thrombosis Diagnosed?
If you or a loved one suspects that you are experiencing symptoms of deep vein thrombosis (DVT), please seek medical treatment immediately. The first step in diagnosing DVT is a thorough medical history and physical examination. Your doctor will ask about your symptoms, risk factors, and any previous medical conditions that might increase your risk of DVT.
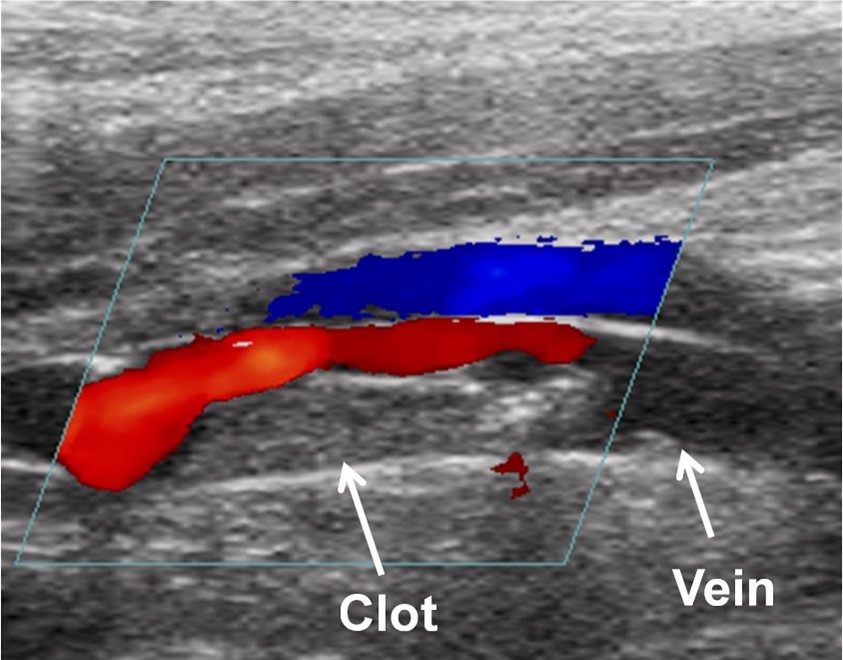
Your vascular specialist will order testing, including lab work and imaging. A D-dimer test (blood test for clot breakdown products), ultrasound (uses sound waves to image blood flow), venography (specialized X-ray with contrast dye), MRI (detailed images of internal structures), or CT venography (CT scan with contrast dye to see blood flow and clots). Ultrasound is the most common due to its effectiveness and safety, while other tests may be used in specific situations.
Diagnosing DVT involves a combination of medical history, physical examination, and various diagnostic tests to detect blood clots and assess the risk of complications accurately. If you experience symptoms or are at risk of DVT, it's crucial to seek medical attention promptly.
Treatment Options for DVT for a comprehensive evaluation.
What are the Treatments for Deep Vein Thrombosis?
Treating DVT involves a combination of diagnostic tests and various treatment options based on the clot's location and severity. The treatment for DVT depends on the clot's location and may include the following:
Compression Stockings
Compression stockings help improve blood flow in your legs and reduce swelling. They are often used if the clot is in the veins below the knee.
Anticoagulants (Blood Thinners)
Anticoagulants are medications that prevent new blood clots from forming and stop existing ones from becoming more significant. They can be taken orally, intravenously (IV), or by injection. Typical treatment lasts 3-6 months, but some patients may need more prolonged treatment.
- Heparin
- Warfarin (Coumadin)
- IVC Filter Placement
- Thrombolysis and Thrombectomy
- Thrombolysis: A medication is delivered directly into the clot to dissolve it.
- Thrombectomy
- Monitoring and Follow-Up
If you have a deep vein thrombosis (DVT) in the veins below your knee, your doctor may suggest regular monitoring with ultrasound scans and compression stockings to prevent the clot from getting bigger or moving. In certain situations, mainly if the DVT occurs repeatedly or without a clear cause, a hematologist may examine you to decide if long-term anticoagulant therapy is needed.
By following your doctor's advice and sticking to the prescribed treatment plan, you can effectively manage DVT and reduce the risk of complications. If you have any questions or concerns about your treatment, do not hesitate to contact a vascular specialist at Center for Vascular Medicine following your DVT treatment.
What Happens if Deep Vein Thrombosis Goes Untreated?
For most patients, a deep vein thrombosis does not go away independently. Most patients will need prescription blood thinners. It is best to seek medical attention when you show signs or symptoms of DVT. Untreated DVT can lead to severe complications, including:
- Pulmonary embolism (PE)
- Post-thrombotic syndrome
- Chronic venous insufficiency
- Increased risk of recurring blood clots
If you experience symptoms, it's essential to seek help, as DVT can cause severe illness and death if left untreated.
DVT Treatment at Center for Vascular Medicine
Deep Vein Thrombosis is a serious condition that requires timely medical attention. Understanding the risk factors, symptoms, and treatment options can help you manage and reduce your risk. If you suspect you have DVT or are at high risk, consult a vascular specialist at Center for Vascular Medicine. Early diagnosis and treatment can prevent complications and improve your quality of life. Find a CVM near you or book a consultation online.
This article is a comprehensive overview of Deep Vein Thrombosis. However, it should not take the place of speaking with a physician. If you are experiencing any of the symptoms listed above, or know someone who is, contact us today to schedule a consultation.
You can also view other vascular diseases below:
Peripheral Arterial Disease (PAD)
FAQs
Yes, in many cases a DVT can be an emergent situation. There is no reason to delay seeking diagnosis and treatment. Never ignore the symptoms and seek medical attention immediately.
In most cases, the answer is no. Most patients will need prescription blood thinners. It is best to seek medical attention when you show signs or symptoms of DVT.
Patient that receive early diagnosis and treatment are more likely to have rapid resolution of their symptoms.
It can be, depending on the size and location of the clot.

