Pelvic pain can arise from various sources, including musculoskeletal problems, ovarian cysts, irritable bowel syndrome, painful bladder, other gynecological issues, and psychological factors. One often overlooked cause of chronic pelvic pain in women is Pelvic Congestion Syndrome (PCS). This condition results from vascular problems in the pelvic region due to improper blood drainage, primarily affecting women who have had multiple childbirths.
What is Pelvic Congestion Syndrome?
Pelvic Congestion Syndrome (PCS) is a vascular disorder involving the veins in the pelvic region. The condition occurs when veins fail to drain blood efficiently, leading to blood pooling and increased pressure in the pelvic veins. PCS is most common in women who have experienced multiple pregnancies. The syndrome must be chronic, lasting six months or more, for a proper diagnosis.
Pelvic congestion syndrome (PCS) is a vascular condition that primarily affects women and is characterized by chronic pelvic pain. This syndrome may be due to dysfunctional veins in the pelvic region, leading to pelvic venous insufficiency and painful symptoms. Symptoms of PCS often include:
Chronic Pelvic, Abdominal, and Lower Extremity Pain
Patients with pelvic congestion syndrome often experience a dull, achy, or pressure-like pain in the lower abdomen and pelvic region that lasts for more than six months. The pain may be constant or intermittent but typically worsens throughout the day. Extended periods of sitting or standing often worsen symptoms, while lying down and elevating the legs can provide relief. Pelvic pain can worsen during or after sexual intercourse (dyspareunia) and menstruation.
Patients with pelvic congestion syndrome may also experience lower back pain, leg pain, and achiness. Lying down or resting often helps relieve the lower abdominal pain caused by pelvic congestion syndrome. Pelvic congestion syndrome can also cause backaches, leg pain, abdominal bloating, and an uncomfortable feeling of heaviness or “fullness” in the pelvic region and lower abdomen.
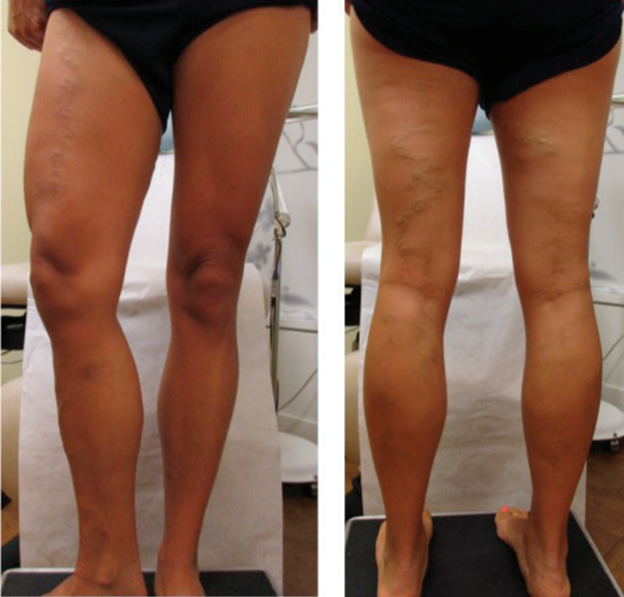
Visible Varicose Veins
Up to 55% of patients with pelvic congestion syndrome experience vulvar varicosities, which are visible varicose veins in the vulva, groin, and surrounding pelvic area. Varicose veins in the pelvic and lower leg region can cause pain, swelling, and discomfort, especially with prolonged sitting or standing. Patients with pelvic varicose veins should talk to their vascular specialist about PCS.
Menstrual Irregularities
Patients suffering from pelvic congestion syndrome may experience severe and painful menstrual cramps (dysmenorrhea) as well as heavy menstrual bleeding (menorrhagia).
What Causes Pelvic Congestion Syndrome?
PCS is caused by increased pressure within the pelvic veins, particularly the ovarian and periuterine veins. When these veins become dilated and fail to drain blood properly, blood pools, raising pressure. Risk factors include multiple pregnancies, births, age, family history, and obesity. PCS often occurs in women with a history of pregnancies, but it can also develop in women with no pregnancy history. Consulting with a vascular surgeon for personalized advice is recommended.
How is Pelvic Congestion Syndrome Diagnosed?
If you are dealing with chronic pelvic pain, pain during sex, or varicose veins in the pelvic area, it's essential to consult a vascular specialist. Early diagnosis and treatment of Pelvic Congestion Syndrome (PCS) can significantly improve your quality of life and alleviate often debilitating symptoms.
PCS is frequently underdiagnosed or confused with premenstrual symptoms, ovarian cysts, uterine fibroids, or other gynecological issues. Because the symptoms of PCS are similar to other gynecological conditions, it's crucial to first work with your primary care provider or gynecologist to rule out any other underlying causes of your pelvic pain before seeking help from a vascular specialist.
The diagnostic process involves a detailed evaluation of the patient's medical history, physical examinations, and various imaging techniques to confirm the presence of PCS and rule out other potential causes of pelvic pain.
Medical History and Symptom Evaluation
The first step in diagnosing PCS is discussing your medical history and symptoms with your vascular specialist. Your vascular specialist will assess the pelvic region and identify any visible signs of varicose veins or swelling. The doctor will palpate the pelvic area to check for tenderness, swelling, or any abnormalities that may indicate PCS. This examination helps in ruling out other potential sources of pelvic pain and guides the physician in selecting appropriate imaging tests.
Imaging Techniques
Imaging is essential in diagnosing pelvic congestion syndrome (PCS). Various techniques are used, including ultrasound, pelvic venography, MRI, CT scan, and IVUS. Ultrasound uses sound waves to visualize pelvic organs and veins. Pelvic venography involves injecting a contrast dye and using X-rays to see pelvic veins. MRI and CT scans create detailed images of the pelvic region. IVUS is a specialized ultrasound technique used to visualize the inside of blood vessels.
Diagnosing Pelvic Congestion Syndrome requires a comprehensive approach that includes a detailed medical history, physical examination, and a combination of imaging techniques to visualize the pelvic veins and identify any abnormalities.
By carefully evaluating all the diagnostic information, physicians can accurately diagnose PCS and develop an effective treatment plan to alleviate the patient's symptoms and improve their quality of life. If you experience chronic pelvic pain or other symptoms of PCS, consult with a board-certified vein specialist to explore your diagnostic and treatment options.
What Makes PCS a Circulatory Problem Instead of an Urinary or a Reproductive Issue?
Not every patient with pelvic pain will be diagnosed with Pelvic Congestion Syndrome. The detailed history of the patient including pregnancies, age, family history, the ultrasound, IVUS examination, and Venography test is evaluated before diagnosing a Pelvic Congestion Syndrome or any other vascular disorder.
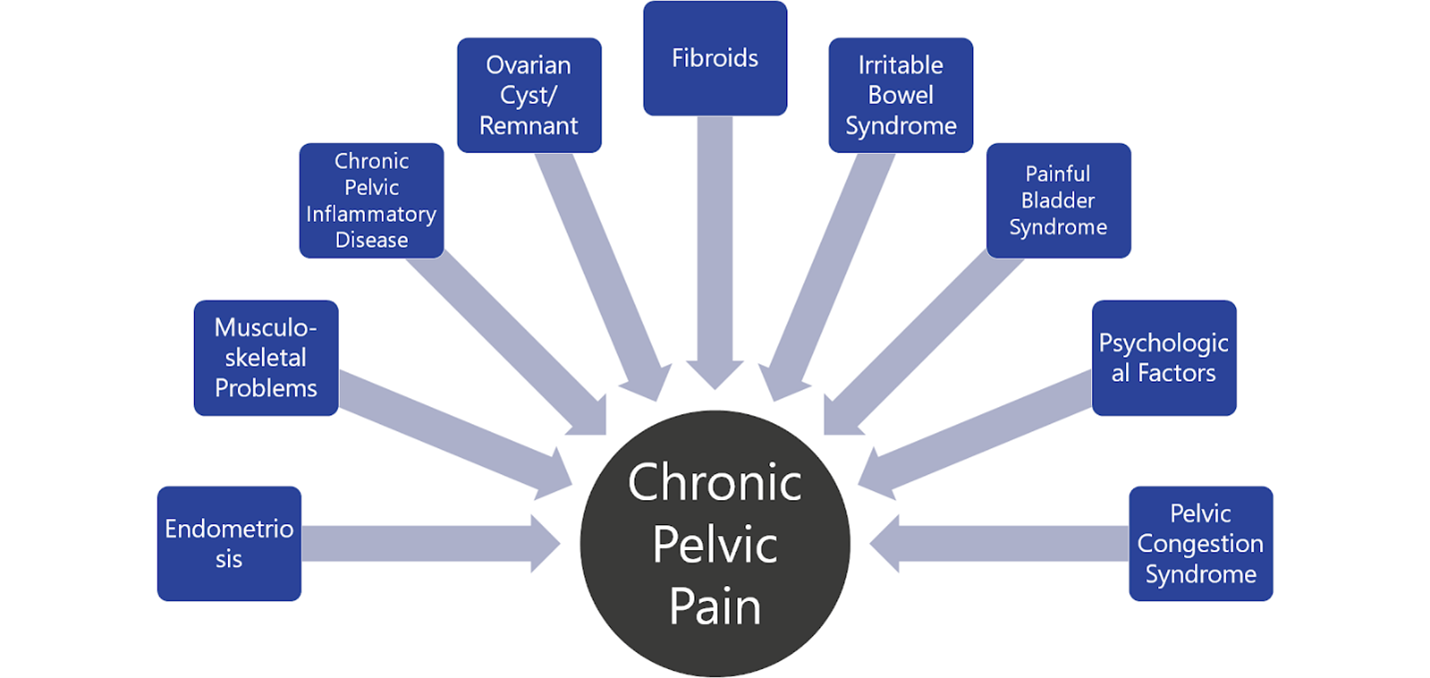
The chart above shows that Chronic Pelvic pain can be caused by a number of disorders and known symptoms. It is up to your physician or a vascular doctor to pinpoint the reason for your pain and improve the quality of your life.
What Are the Treatment Options for Pelvic Congestion Syndrome?
Managing PCS can be difficult, but several effective treatment options are available. These include conservative management and self-care, as well as advanced minimally invasive procedures. The goal of treatment is to relieve symptoms, improve quality of life, and prevent potential complications associated with PCS.
Conservative Management and Self-Care
Initial treatment for PCS often involves conservative management and self-care measures. These non-invasive approaches can help manage symptoms and improve overall comfort.
Compression Garments
Wearing medical-grade compression garments, such as compression pantyhose or shorts, can help improve blood flow in the pelvic region. These garments provide external pressure that supports the veins, reducing blood pooling and alleviating symptoms of discomfort and swelling.
Pain Relief Medication
Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce inflammation and alleviate pain associated with PCS. These medications are often recommended for managing chronic pelvic pain and painful menstrual cycles.
Hormonal Therapy
Hormonal therapy may be prescribed by a gynecologist or primary care provider to help manage PCS symptoms. Estrogen levels can influence the development and severity of PCS, and hormonal treatments can help regulate these levels to reduce symptoms. Birth control pills, hormone replacement therapy, or other hormonal medications may be used depending on the patient's specific needs.
Outcomes of treatment allows patient to regain quality of life and may prevent need for more invasive surgical treatment such as hysterectomy. Expectations of treatment is to relieve chronic pelvic pain especially when it is related to certain activities of daily living. The goal is to also relieve symptoms of pain during/after sexual activity(dyspareunia), painful menstrual cycles(dysmenorrhea) and reduce prominent varicose veins in the vaginal and genital region(s).
In the video below, Dr. Satwah explains Pelvic Congestion Syndrome along with a case study.
Can I Prevent Pelvic Congestion Syndrome?
Your vascular health isn’t limited to just one part of your body. Maintaining healthy habits and lifestyle changes can help you reduce your risk of developing PCS and other venous conditions. Preventing PCS entirely may not always be possible, as many factors are outside the patient’s control. Still, there are steps you can take to help alleviate symptoms, reduce your risk, and improve your overall vascular health.
Maintain a Healthy Weight
Maintaining a healthy weight is crucial for reducing pressure on your vascular system and lessening your risk of developing diabetes and high blood pressure. Both of these can cause weakened vein walls that lead to varicose veins in the lower extremities and throughout the body.
Focus on a Healthy Diet
Make healthy dietary choices, including high-fiber, heart-healthy foods like fruits, vegetables, leafy greens, and lean protein like chicken or fish. Stay hydrated and try to limit salty foods that can cause dehydration.
Stay Active
Regular physical activity helps to keep your vascular system strong, reduces inflammation and swelling, and prevents blood from pooling in the lower extremities. While specific exercises like weight lifting and cycling can worsen pelvic congestion symptoms, low-impact cardio exercises such as swimming, walking, yoga, and pilates can strengthen the pelvic muscles and improve circulation, promoting healthy veins and overall wellness.
Positive Lifestyle Changes
Incorporating healthy lifestyle changes can help improve your vascular health and potentially reduce your risk of PCS. Decrease your alcohol consumption and talk to your provider about finding support to quit smoking.
Keep a Healthy Sleep Schedule
Remember to maintain a healthy sleep schedule. Adequate and regular sleep can improve overall circulation, essential for those with Pelvic Congestion Syndrome (PCS). Poor sleep can lead to increased stress and inflammation in the body, worsening vascular issues, including those in the pelvic region. Getting sufficient, quality sleep helps your body maintain optimal blood flow, reducing the likelihood of blood pooling in the pelvic veins.
Wear Compression Garments
Compression garments are an excellent non-invasive treatment for managing and relieving Pelvic Congestion Syndrome (PCS) symptoms. These garments apply external pressure to support the veins in the pelvic region, which helps improve blood flow and reduce blood pooling that leads to PCS.
Compression garments consistently apply pressure to the pelvic area, enhancing blood flow. The pressure from these garments supports the veins, helping them push blood back towards the heart more effectively. This is especially helpful for those with PCS, as it prevents blood from pooling in the pelvic veins, reducing congestion and symptoms.
Compression therapy isn’t for everyone; discuss compression therapy with your vascular specialist before purchasing or wearing compression garments.
Pelvic Congestion Syndrome Treatment and Diagnosis with Center for Vascular Medicine
Pelvic Congestion Syndrome can cause chronic and sometimes debilitating pain, affecting daily life. Early detection and treatment are crucial for managing symptoms and improving quality of life. Center for Vascular Medicine offers comprehensive care for PCS, helping patients regain their health and well-being. If you experience PCS symptoms, consult our board-certified vein specialists to explore your treatment options. Make an appointment or find a Center for Vascular Medicine near you!
You can also view articles related to this condition:
Top Warning Sign of Lower Abdomen Pain After Sex
The Female Patient Guide for Pelvic Pain Specialists
FAQs
Many of our referring physicians and patients ask fantastic questions regarding this disease. Some of the frequently asked questions (FAQ), and our answers are below.
Other treatment options include more invasive surgical options of hysterectomy. During a hysterectomy the periuterine veins are typically removed at the same time. Risks and recovery from hysterectomy are elevated with more invasive surgical procedures
Here is how our patients describe their pelvic pain…
- I have had pelvic pain for a very long time and none of my doctors are sure of what is going on.
- I feel bloated all of the time.
- My pain in my pelvis gets worse when I am standing for a long time and I have to lay down.
- I feel like I have a lot of pressure in my “private area”
- I get swelling in my “private area”
- I feel like a bowling ball is stuck in my groin area.
- I feel like I have a bladder infection all of the time
- I don’t want to have any sexual relationships because of the pain that I have with it
- I have always had very painful and heavy periods that stop me from being able to do what I want or need to do
- My doctor has told me that I have “bulging veins” or varicose vein in my vagina.
- I feel very frustrated that I have gone to so many doctors and I feel like they don’t believe me and they cannot tell me what is causing my pain
There are different reasons for pelvic congestion & pain. Pelvic Congestion Syndrome is a chronic pelvic condition usually lasting more than 6 months. A proper pelvic ultrasound and comprehensive questionnaire will help determine if you have the disorder. Please call one of our physician offices to help you with diagnosis and a detailed evaluation.
Pelvic Congestion Syndrome is commonly misdiagnosed and underdiagnosed. It occurs most commonly in women 20-50 and is typically diagnosed after multiple pregnancies. It is estimated to occur in approximately 15% of women in the US.
Success Stories of Patients

