What is Restless Legs Syndrome?
Restless Leg Syndrome, or RLS, may be more common than you know. RLS is found in approximately 5 to 10 percent of adults in the United States and affects women more than men. It also seems to worsen as a person gets older. So, how do you treat it, and what causes it?
What is Classified as Restless Legs?
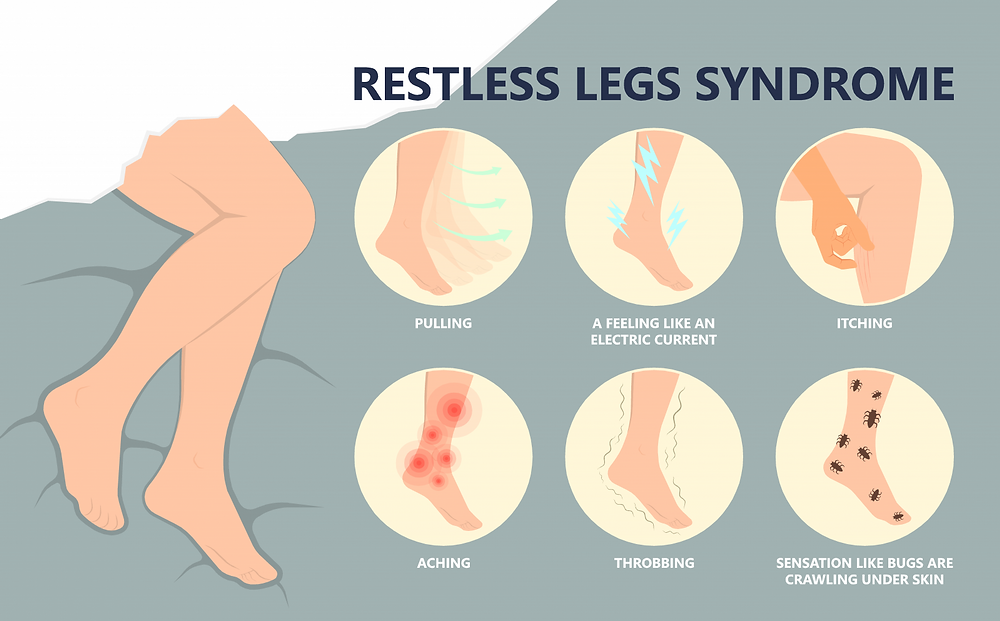
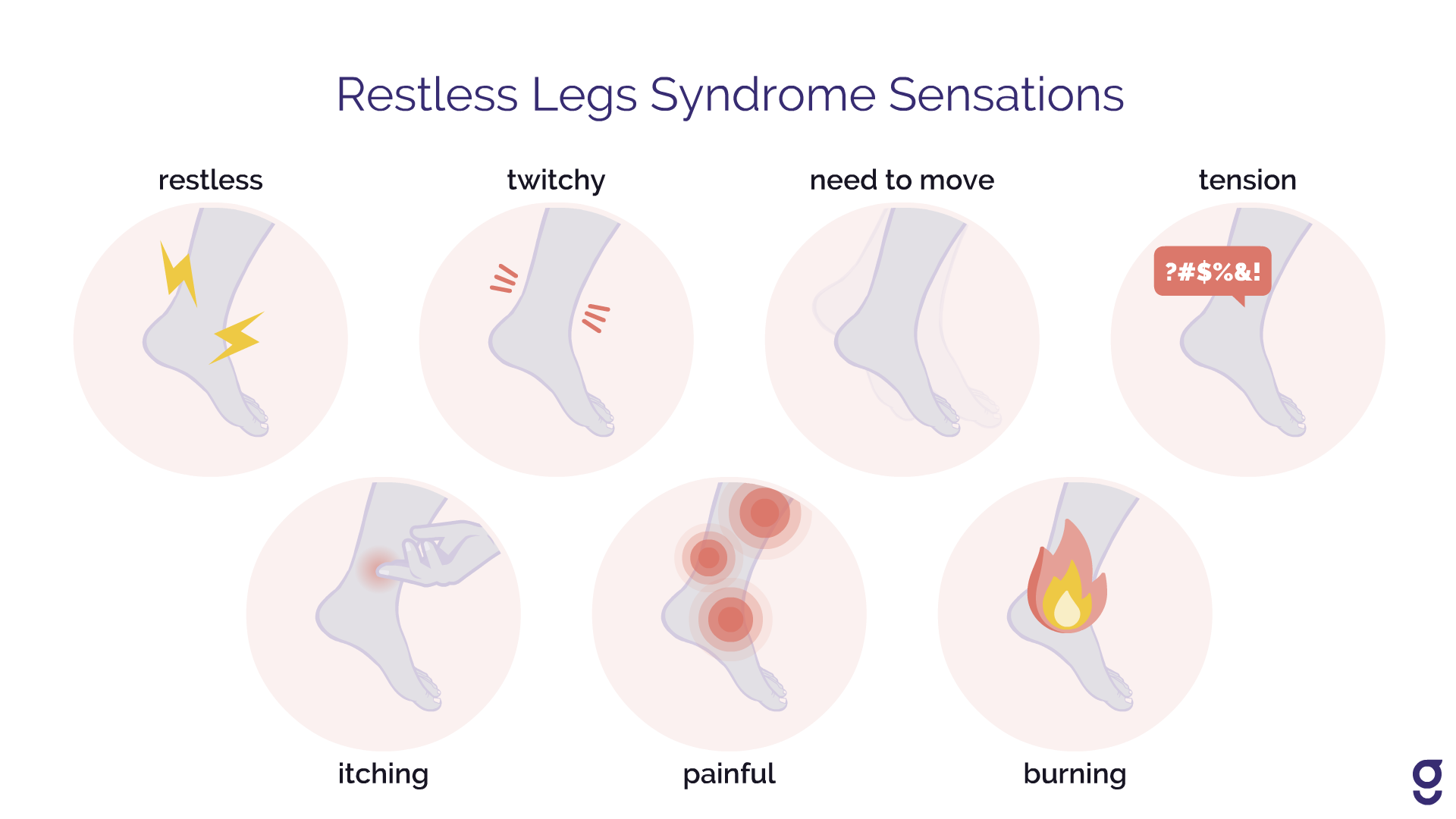
RLS is an overwhelming urge to move your legs due to unbearable sensations. Restless Legs Syndrome treatments range from conservative, at-home remedies for mild to moderate symptoms to surgical or pharmaceutical interventions for severe symptoms.
While there is no exact cause of Restless Leg Syndrome, some researchers feel the following factors may play a part in it:
- Chronic Disease
- Pregnancy
- Genetics
- Medications
- Poor circulation in lower extremities
People with RLS claim the sensation feels like crawling, tingling, or aching pain that finds release by moving the legs. RLS tends to get worse towards the evening and can cause sleeplessness and fatigue.
Treating Restless Legs
Step-by-step Guide to Treating Restless Legs Caused by a Vascular Disease
Restless Leg Syndrome symptoms usually don’t occur during the day and, in some cases, only happen intermittently at night. There may be several months with no signs before it starts up again.
For these reasons, many people don’t follow-up with their healthcare provider. However, it’s essential to do so. There may be underlying medical issues causing the RLS, and by treating the root cause, people may see an improvement in their condition.
During your exam, your physician may check your pulse in your legs. A weak or absent pulse could be an indication of vascular disease. If you discover that you have vascular disease, then you must follow up with a physician whose specialty is vascular medicine. The medical staff at the Center for Vascular Medicine (CVM) specialize in vascular disease and can help you find relief. Here is what you can expect during your appointment at the Center for Vascular Medicine:
Diagnosis
Your physician will likely order a comprehensive diagnostic test to check for vascular diseases, such as an ABI (ankle-brachial index) or ultrasound scan. Depending upon your results, there are different options for treatment based on the severity of the disease.
Treatment options
The good news is that RLS doesn't have to be forever - here are some common treatment options that may help:
Conservative treatment for restless legs involves compression therapy. Compression bandages are wrapped around the lower leg, applying constant pressure to the affected area. These bandages will help improve circulation by pushing the blood through the veins.
Many people have found relief from Restless Leg Syndrome with hot and cold compresses, especially when they alternate between the two. Additionally, applying magnesium to your lower legs may also help to alleviate the symptoms.
Your doctor may recommend surgery to address the disease. There are a few surgical options for treating restless legs due to vascular disease, and most surgeries are non-invasive and may involve stenting, angioplasty, or by-pass surgery.
Prognosis
Combining medical interventions with lifestyle changes offers the best chance to relieve the symptoms of Restless Leg Syndrome caused by vascular disease. A healthy diet, moderate exercise, and stress management are essential to good long-term outcomes.
Think you may have vascular symptoms of Restless Legs?
Non-Drug Treatment
People can treat Restless Leg Syndrome without pharmacological intervention. A hot bath may help alleviate the symptoms, especially when combined with Epsom salts or essential oils.
Massaging the legs may also provide relief. Try rubbing your calves in the evening, maybe while watching television before bed. Using a foam roller or deep tissue massage will help your lower legs with blood circulation. One study showed that regular massage therapy helped decrease the symptoms of RLS.
You might want to consider stretching and yoga as a non-pharmaceutical approach to RLS. Both of these can decrease the severity of the symptoms. Calf stretches, hamstring stretches, and forward folds have helped many people who suffer from RLS.
Yoga can also help to relieve stress, a factor that many feel to be a contributing factor to RLS.
Lifestyle Changes to Decrease Symptoms of Restless Legs
Sometimes changes in your lifestyle can aid you in managing the symptoms of RLS. The following may help:
Exercise
Keeping your body active may be beneficial in managing symptoms. It doesn’t have to be high-intensity, and you shouldn’t overdo it, but adding regular movement throughout the day can help.
Diet
Adding and removing certain foods have been shown to help those who suffer from RLS. Try adding foods to your diet that are rich in iron, folate, and magnesium. Some examples are red meat, spinach, almonds, cashews, brown rice, and avocados.
It would be best if you tried to avoid caffeine. Caffeine is a stimulant and may make it harder to sleep at night. Sources of caffeine include coffee, tea, soda, and chocolate.
Quit Smoking and Avoid Alcohol
Both smoking and alcohol can trigger or worsen the symptoms of Restless Leg Syndrome. Either quitting or cutting down on both of these may help relieve the pain.
Iron Supplementation
One common cause of Restless Leg Syndrome is iron deficiency (anemia). In addition to RLS, many people with anemia also feel chronic fatigue and have shortness of breath. A complete blood count (CBC) test will determine if your red blood cell count is low. If that is the case, your healthcare provider may suggest adding an iron supplement to your diet.
Common Drugs to Treat Restless Legs
Currently, there are four drugs approved by the U.S. Food and Drug Administration (FDA) to treat moderate to severe cases Restless Leg Syndrome. Two of them work to stimulate the brain’s dopamine receptors, and the other two work to block nerve pain.
Depending on other symptoms you have with RLS, your physician may prescribe one of these:
- Ropinirole (dopamine promoter)
- Pramipexole (dopamine promoter)
- Gabapentin (nerve pain)
- Pregabalin (nerve pain)
What to Expect after Treatment with CVM
The caring and compassionate staff are committed to your long-term health and wellbeing. That’s why after receiving treatment with the healthcare team at CVM, we will follow up with you at intervals post-procedure. These dates are flexible depending on your medical needs, but will typically follow this schedule:
One to Two Weeks
The first couple of weeks are critical, so you'll typically go through these stages:
- Discussion of the procedure
- Checking for a decrease in symptoms
- Complications, if any
- Intraoperative imaging
Six Weeks
At six weeks, we'll:
- Continue to monitor for improvement
- Ensure there are no issues with anticoagulation medication
- Possibly order an ultrasound
Three Months
After three months, you can expect us to:
- Order an ultrasound, if one wasn’t done at six weeks
- Discuss the ending of your anticoagulation therapy
- Continue to monitor for improvement
Six Months (and Every Six Months After That)
Your healthcare provider will continue to monitor your progress to ensure improvement and ensure no other problems arise.
Even if your physician chooses to treat your RLS conservatively without surgical intervention, you will still be asked to follow-up between three months and one year to monitor improvement or worsening symptoms.
If you’ve been suffering from Restless Leg Syndrome, call your closest CVM and schedule your appointment today.
Restless Legs Syndrome Foundation is an excellent source for anyone who has RLS or wants to learn more about its symptoms, treatments, and the latest research.
Ready to speak with a vascular specialist?

